Pre-reading
| Site: | TAFE SA Learn |
| Course: | Community Services and Health First Aid |
| Book: | Pre-reading |
| Printed by: | Guest user |
| Date: | Tuesday, 23 September 2025, 1:33 AM |
Table of contents
- Introduction
- What is First Aid?
- How to Recognise and Respond to an Emergency
- Australian Emergency Services
- Alternative Mobile phone number
- Legal Considerations for First Aid
- Standard Precautions and Cross Infection Risks
- First Aid Kits
- Recording and Reporting
- Traumatic Incident Stress
- How to Protect Yourself from Incident Stress
- Assessment of an Emergency: Primary and Secondary Surveys
- D = Check for Danger
- R = CHECK FOR REPONSE
- S = SEND FOR HELP
- A = AIRWAY
- B = BREATHING
- C = Cardiopulmonary Resuscitation [CPR]
- D = Defibrillation
- Cardiopulmonary Resuscitation (CPR)
- The Unconscious Casualty
- Secondary Survey
Introduction
Accidents or sudden illness usually occur with little or no warning and can happen in any environment, at any time. Accidents or sudden illness can result in minor injury or sudden loss of life. Accidents can involve just one person or many hundreds of people whilst at home, work or at social or recreational activity.
The effects of an injury or sudden illness can last from hours to a lifetime.
Most accidents can and should be prevented.
![]() The Australian Resuscitation Council website is an important policy and guidelines resource for this course. You can bookmark it for ongoing reference.
The Australian Resuscitation Council website is an important policy and guidelines resource for this course. You can bookmark it for ongoing reference.
What is First Aid?
- Preserve Life
- Prevent further injury
- Promote recovery by providing initial management that may reduce the impact of any injuries already sustained by a casualty.
- Protect the unconscious
- Seek medical assistance
How to Recognise and Respond to an Emergency
A medical emergency could be when a person becomes unconscious or suffers a heart attack or stroke. An injury is when damage occurs to some part of a person’s body, for example a broken bone or deep cut that bleeds freely.
How to respond to an EmergencyYou can always do something to help.
Remain calm and communicate with others involved in the emergency. Remember to:
-
- call 000 or ask someone else to
- make the area safe, for you, any bystanders and the casualty
- assess the casualty’s care needs and commence appropriate management
- record all relevant information about the emergency.
Australian Emergency Services
 Once connected you will be asked a series of questions, remain calm and answer all questions carefully. An emergency vehicle will be dispatched as soon as the operator knows the location and the type of assistance you require. Don’t hang up until told to do so.
Once connected you will be asked a series of questions, remain calm and answer all questions carefully. An emergency vehicle will be dispatched as soon as the operator knows the location and the type of assistance you require. Don’t hang up until told to do so.Some of the questions you may be asked include:
-
- your location, don’t forget to include landmarks where necessary
- the nature of your emergency, what type of accident or illness has occurred and a brief description of what has happened
- the number of people affected by the emergency and the nature of their injuries
- your name and the phone number that you are calling from.
Depending on the emergency the operator may provide you with step-by-step assistance on how to provide initial first aid management, this assistance can continue until the emergency vehicle arrives. All emergency calls are recorded.
Alternative Mobile phone number
The ICE contact number is to be used by specific medical professionals only.
| OTHER USEFUL PHONE NUMBERS | |
| Police assistance, other than in an emergency | 13 14 44 |
| Australian Medic Alert Foundation | 1800 882 222 |
| Ambulance/Fire/Police | 000 |
| Poisons Information Centre | 13 11 26 |
| Alcohol & Drug Information Service | 1800 422 599 |
| Kids Help Line | 1800 551 800 |
| Heart Foundation | 1300 362 787 |
| Anaphylaxis Australia | 1300 728 000 |
| Asthma Australia | 1800 645 130 |
| Diabetes Australia | 1300 136 588 |
| Beyond Blue | 1300 224 636 |
| Life Line | 13 11 14 |
Legal Considerations for First Aid
When you provide first aid, based on your up to date training, you have nothing to fear legally in helping another person. The general legal principle is that a person who renders first aid is expected to act reasonably and with a genuine concern for the best interest for the casualty.
As a trained first aider you are expected to provide assistance based on the Australian Resuscitation Council policies and protocols; in doing so you will have nothing to fear when you help another person in an emergency. Always gain consent from a conscious casualty prior to rendering first aid, consent may be assumed from a person who is unconscious.
Further discussion on legal considerations including Duty of Care and Negligence will occur during practical sessions.
Standard Precautions and Cross Infection Risks
- Wash and dry your hands before and after contact with the casualty
- Use protective barriers when necessary, which may include gloves, gowns, mask
- Use aprons, masks, eye shields or goggles
- Use protective barriers when performing resuscitation
- Use appropriate handling and disposal techniques for contaminated waste products.

First Aid Kits

Keep well stocked first aid kits in your home, vehicle(s) and workplace. Ready-made first aid kits can be purchased from a range of suppliers.
A well-stocked first aid kit should include:
-
- disposable gloves
- resuscitation face shield or mask
- dressings; a range of non-adherent and gauze dressings and adhesive strips
- bandages; a range of conforming and crepe roller bandages, triangular bandages and eye pads
- hypoallergenic tape, a pair of scissors, tweezers and safety pins
- alfoil rescue blanket
- safety glasses
- pen and note pad.
Do not keep medicines or liquids in the first aid kit. All kits should be kept in a safe, secure place out of reach of children.
Recording and Reporting
It is necessary to record and report details of any first aid incident. As soon as possible the first aider should collect, collate and document as much relevant information about the casualty(s) as possible and should include:
-
- a detailed history of the incident, (what happened, when, how and why)
- a description of the first aid management of injury/illness, including the use of any form of medication and the giving of food/fluid
- the time, date and location of incident
- people involved in the incident, include your name and contact details.
Follow general documentation principles: Write clearly in pen
-
- Use simple, non-jargonistic terms
- Do not obliterate any words or sentences, if a mistake is made strike a single line through the error, initial the mistake and continue
- Sign, date and witness the report
- Always maintain confidentiality and provide reports to health care professionals, on a need-to-know basis.
Traumatic Incident Stress
Traumatic incidents can produce unusually strong emotional reactions that may interfere with your ability to function either at the time of the incident or sometime later.
A first aider may experience physical, cognitive, emotional or behavioural reactions including:
| Physical | Cognitive | Emotional | Behavioural |
|
Difficulty breathing * Chest pain * Fatigue Dizziness Nausea/vomiting Thirst Visual disturbances |
Confusion, poor concentration, disorientation Memory difficulties Poor problem solving Nightmares |
Anxiety Guilt, grief or denial Fear Irritability Loss of emotional control Feeling overwhelmed Blaming self or others Depression |
Anger Withdrawal Emotional outburst(s) Alteration in appetite Excessive use of drugs or alcohol Inability to rest |
| * If you experience any of these symptoms, seek immediate medical assistance. | |||
How to Protect Yourself from Incident Stress
Remember that strong emotions are NORMAL reactions to abnormal situations!
-
- Take care of yourself: Stay focused on hazards at the incident site and keep vigilant about your safety.
- Don’t expect too much of yourself, do what you can as well as you can.
- Approach the site calmly, do not run, take deep calming breaths as needed.
- Always aim to work as a team with other first aiders and emergency personnel.
- Step back as soon as you can, let others take over the care when appropriate.
- Get professional help: speak to emergency personnel at the time of the incident, seek support from medical professionals and/or contact support agencies like Life Line 13 11 14.
Once at home and over time, your impressions and understanding of your experience will change; this is different for everyone. If, after several weeks you are experiencing signs and/or symptom of Traumatic Incident Stress, obtain professional help.
Assessment of an Emergency: Primary and Secondary Surveys
PRIMARY SURVEY:
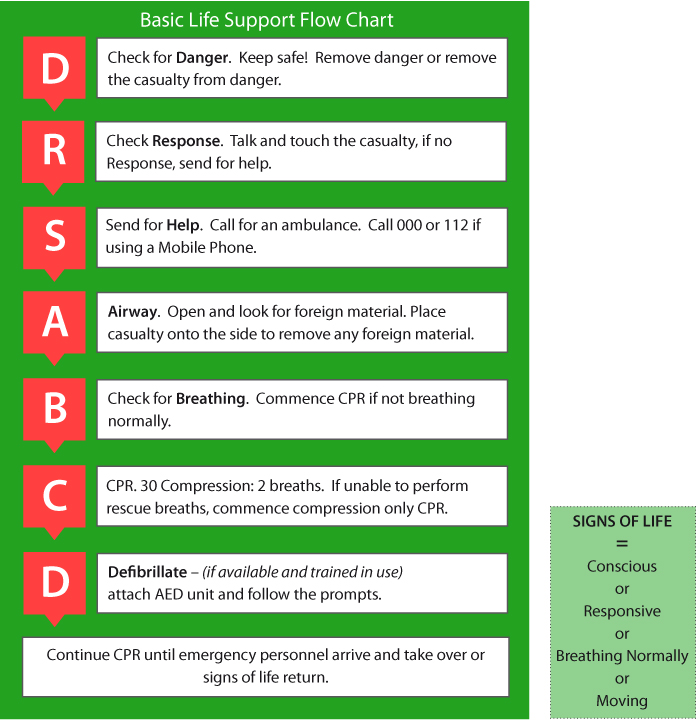
D = Check for Danger

Protect yourself, bystanders and the casualty from further injury.
DO NOT APPROACH IF TOO DANGEROUS
For example an area with an explosive potential or close to fallen power lines. Maintain a safe distance, call emergency services (000) and warn others of the danger.
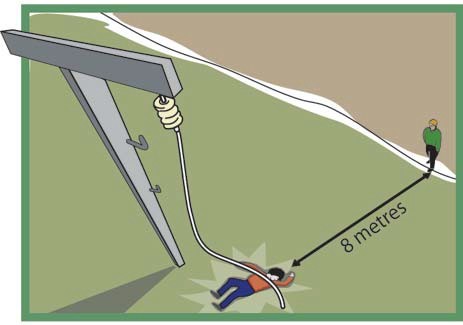
If the danger can be managed, then initially aim to remove the danger or, if this is not possible, then move yourself and the casualty to a safe area as quickly as possible. If an injured person cannot shift themselves independently you could attempt to drag the person, by their feet or arms, to a safe area. Ideally avoid bending, twisting or carrying the casualty.
R = CHECK FOR REPONSE

 |
 |
Talk and Touch
Approach the casualty, speak in a calm clear manner, identify yourself by name and ask if you can help. For example ‘Hello, my name is Scott Williams, can I help you?’ Gently touch the casualty on the lower leg, hip and/or shoulder and ask ‘what is your name’ or ‘open your eyes’.
If the casualty RESPONDS then check for severe bleeding, if present treat the bleeding and then undertake a secondary survey.
If the casualty DOES NOT RESPOND Call 000 or 112, if you have not already done so and continue with the primary survey.
S = SEND FOR HELP


Call 000 or mobile number 112 for an ambulance or ask a bystander to make the call.
A = AIRWAY

 |
 |
 |
| Adult | Child | Infant |
Open the casualty’s mouth and look inside; if clear of any foreign debris, check for breathing.
-
- If foreign debris is present; reposition the casualty’s head or body to one side and sweep any debris from the mouth with gloved fingers.
- Leave well-fitting dentures in place.
Once the airway is clear, continue with the primary survey.
B = BREATHING


Place one hand over the casualty’s mouth and nose and the other on their lower chest area, can you SEE movement? Can you FEEL air coming from the casualty’s mouth or nose? Can you HEAR sounds of breathing?
YES, the casualty IS breathing:

Position the casualty onto their side, if not already in that position, check for severe bleeding, undertake a secondary survey and continue to monitor the casualty’s airway and breathing every minute or two until emergency personnel arrive.
If there are NO signs of life – no response, absent or inadequate breathing, no movement – start immediately with 30 chest compressions.
-
- Position the casualty onto their back, if not already in that position.
C = Cardiopulmonary Resuscitation [CPR]


Position the casualty on their back on a firm, flat surface.
Locate the centre of the chest.
Use 2 hands: deliver 30 compressions at a rate of approximately 100–120 compressions per minute, that is almost 2 compressions every second!
Depression depth is approximately one third of the chest depth, which is about 5 to 7 cm in an adult.
Give 2 breaths (use barrier mask if available), check to see inflation of the lungs. If the chest does not rise ensure you have appropriate backwards head tilt and jaw lift and an adequate air seal by covering all of the casualty’s mouth and sealing the nose with your fingers or cheek.
Continue to deliver 30 compressions followed by 2 breaths until an ambulance arrives, the casualty recovers or the first aider is unable to continue, usually due to physical exhaustion.
If unwilling /unable to perform rescue breaths continue chest compresions.
For a person using the Symbicort (Symbicort as both reliever and preventer) SMART program a special first aid management plan exists that does not use a blue reliever. However, if the casualty does not have a Symbicort inhaler available then follow the Asthma 4 x 4 first aid response steps.
D = Defibrillation

Defibrillation Using an Automated External Defibrillator [AED]

If AED is available and the first aider is trained in defibrillator use:
-
- Check the AED is charged and in operational order
- Expose the chest, dry and/or shave excessive hair if necessary
- Attach chest pads onto dry chest as illustrated on AED unit
- Follow the voice prompts.
Cardiopulmonary Resuscitation (CPR)
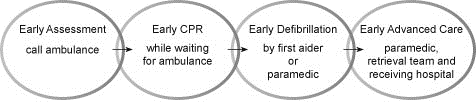
CPR is the combination of chest compressions and breaths and is conducted on a non-responsive casualty who is not breathing properly.
Studies have shown that most cardiac arrest casualties die before reaching hospital and that about 80 percent of cardiac arrests occur in the home. Early recognition, immediate and continuous CPR, early defibrillation and early advanced medical care all contribute to an improved survival rate.
CPR will help to bridge the gap between the casualty collapsing and the arrival of an ambulance or other medical personnel. Remember any CPR is better than no CPR at all.
Cardiopulmonary Resuscitation CPR for Infants and Children
Although the CPR ratio of 30 compressions: 2 breaths and the compression location, depth and rate does not change regardless of the age of the casualty there are some important points to consider when providing CPR for infants or children.
Use two fingers to compress the chest in an infant and two hands for a child, use less pressure than for an adult.

Infants and small children do not require the same backwards head tilt and jaw lift as adults. Deliver only small ‘puffs’ of air to an infant with their head in a neutral position.
Breaths can be delivered by blowing gently into the nose and mouth or just the nose.
In class based contact you will be shown the different head position, jaw support, barrier mask use and compression techniques for the resuscitation of babies and children.
Remember when you approach any emergency incident, assess the situation carefully. Ask yourself the following questions.
-
- What has happened? (try asking the casualty or bystanders).
- Is the area safe?
- How many people are injured or ill?
- What is the extent of any injuries or illness?
- What sort of help are you going to need?
It is essential that all first aiders work together as a TEAM.
Involve other trained first aiders and bystanders in the care of any injured or ill casualties. Delegate tasks to confident bystanders, for example ask that they call emergency services or provide first aid materials like first aid kits, blankets or pillows.
The Unconscious Casualty
A person is considered unconscious if they are unable to:
-
- respond to your spoken word or gentle touch.
Unconsciousness can be caused by:
-
- direct head or neck trauma
- overdose of drugs or alcohol electric shock
- alteration in blood pressure
- a medical emergency like stroke, poorly controlled diabetes or a seizure
- many other emergencies.
An unconscious casualty is at risk of death if left on their back or slumped in such a way as to block their airway.
Management of an Unconscious Casualty
- DRSABCD
- If breathing adequately place the casualty onto their side in a Airway Protected Position
- Check and control any severe bleeding
- Check for other injuries
- Stay with the casualty until help arrives
- Monitor and note any changes in the casualty’s condition and report this information to the attending emergency or medical personnel.
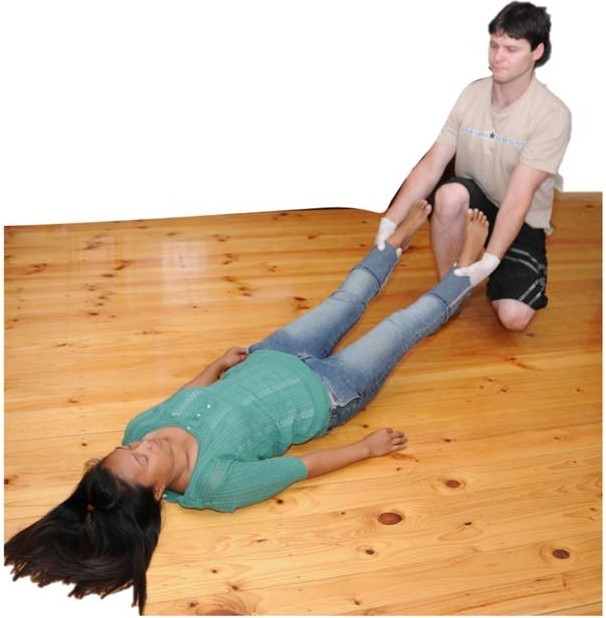
The Airway Protected Position (also known as the coma, stable side and recovery position)
The semi or unconscious casualty must be positioned on their side to protect their airway from becoming blocked.

Position a pregnant woman onto her left side

- While kneeling, place the person’s arm furthest from you to 90 degrees
- Bring the knee closest to you up to a fully bent position
- Place the arm closest to you across the person’s chest, fingers pointing to shoulder area
- Gently roll the person away from you
- Limit further movement by keeping the uppermost leg at a right angle to and touching the ground
- To protect the airway, position the person’s mouth towards the ground
- Recheck the casualty’s breathing, Look, Listen and Feel for adequate breathing
- Check for and control blood loss and manage any visible injuries
- Continue to monitor the person until emergency personnel arrive.
Secondary Survey
Undertake a SECONDARY SURVEY when:
-
- the casualty is in a safe area
- the casualty is fully conscious and able to respond to your questions, and
- if possible, you have access to a First Aid Kit and applied Personal Protective Equipment such as gloves and safety glasses.
Steps to conduct a secondary survey - Look for signs and symptoms of injury or illness.
1. Ask the casualty:
- What happened; how did it happen, when and why did it occur?
- How do they feel now, do they have pain?
- Do they have a known medical condition?
- Do they take any medications?
- Look for anything abnormal.
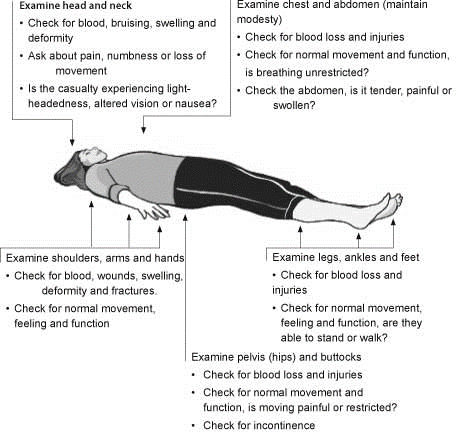
- Continue to monitor breathing, pulse, colour, warmth and movement.
3. Treat any injuries:
- Control severe blood loss as soon as possible and call 000 or 112.
- Treat other injuries and obtain medical assistance as soon as possible.